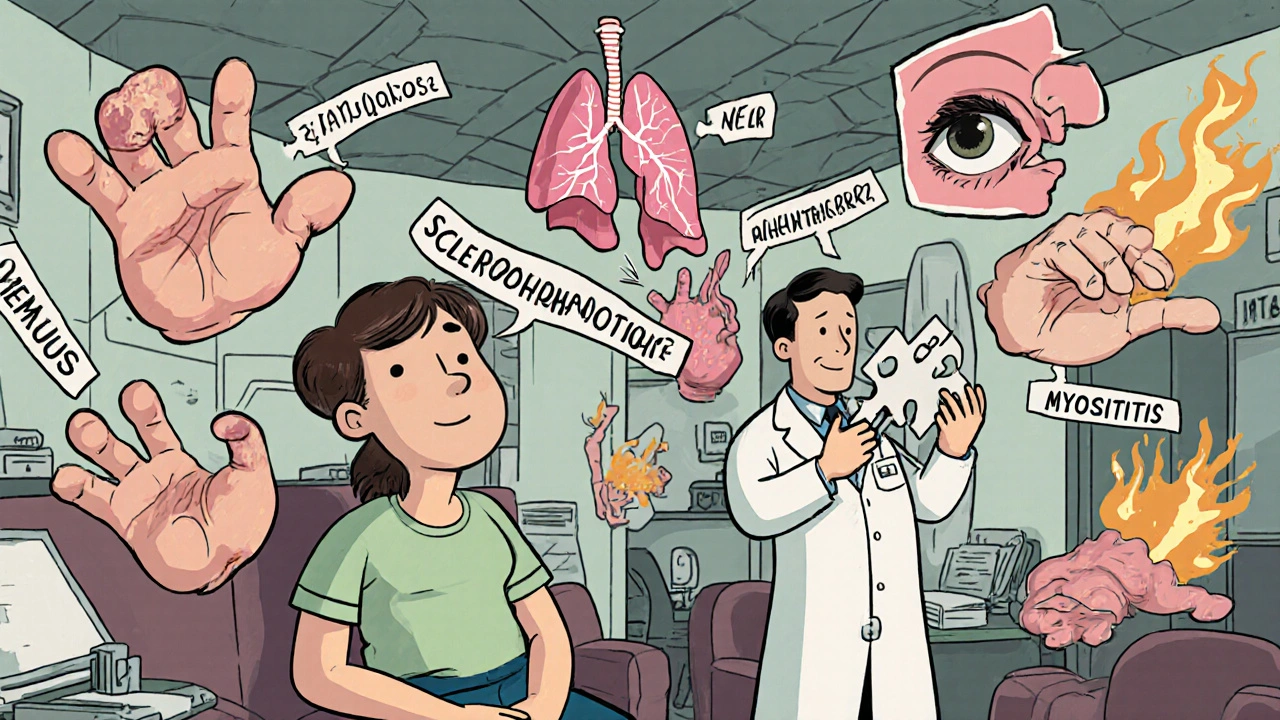
Imagine being told you have lupus, then months later, your fingers start tightening like rubber bands. Your muscles ache, your lungs feel stiff, and your eyes burn constantly. Your rheumatologist says it’s scleroderma now. Then your pulmonologist mentions interstitial lung disease. You’re seeing five different specialists, each treating one piece of you-but no one is putting it all together. This isn’t rare. It’s autoimmune overlap syndromes.
What Exactly Are Autoimmune Overlap Syndromes?
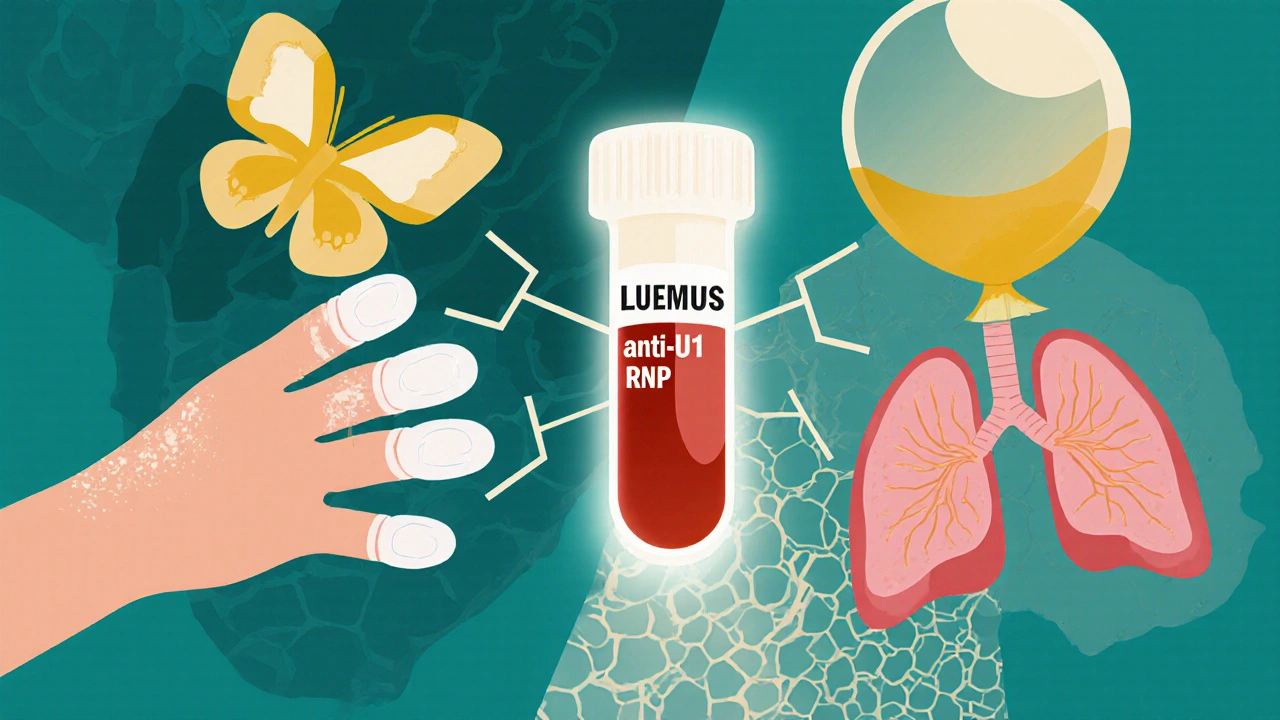
Autoimmune overlap syndromes happen when a person’s immune system attacks more than one part of the body at the same time, meeting diagnostic criteria for two or more distinct autoimmune diseases. These aren’t just random combinations. They follow recognizable patterns. The most common are mixed connective tissue disease (MCTD), antisynthetase syndrome, and polymyositis/scleroderma (PM/Scl) overlap.MCTD, first identified in the 1970s, shows up with a signature antibody: anti-U1-RNP. People with this often have puffy hands, Raynaud’s (fingers turning white in the cold), swollen joints, and muscle weakness-all symptoms that look like lupus, scleroderma, or myositis, but together. Up to 95% of MCTD patients have Raynaud’s. That’s not a coincidence. It’s a clue.
Antisynthetase syndrome is different. It’s tied to antibodies against enzymes that help build proteins in cells. The most common is anti-Jo-1. These patients don’t just have muscle pain-they often develop serious lung scarring (interstitial lung disease) and rough, cracked skin on their fingers called mechanic’s hands. About 65% of them have lung involvement. If you’re diagnosed with myositis and suddenly start coughing, this is the red flag.
PM/Scl overlap is less talked about but just as real. Patients have skin thickening like scleroderma, but also muscle weakness like polymyositis. Their antibody profile? Anti-PM/Scl. It’s rare-only 2-5% of scleroderma patients have it-but when you see both skin tightening and muscle inflammation together, this is what you’re looking for.
And then there’s Multiple Autoimmune Syndrome (MAS), where three or more autoimmune diseases cluster in one person. This can include Sjögren’s, rheumatoid arthritis, thyroid disease, and even type 1 diabetes. It’s not random. There’s a genetic and immune pattern tying them together.
Why Diagnosis Takes So Long
The problem isn’t that doctors don’t know these syndromes exist. It’s that the rules for diagnosing them are messy. The American College of Rheumatology and European League Against Rheumatism have clear criteria for lupus, scleroderma, or myositis individually. But there’s no official checklist for when they overlap.As a result, 30-40% of patients start out labeled with “undifferentiated connective tissue disease” (UCTD)-a fancy way of saying, “We see something, but we can’t name it.” Over five years, nearly half of those UCTD patients end up with a clear overlap diagnosis.
Patients often wait 18 months or longer to get the right label. Compare that to 12 months for a single autoimmune disease. Why? Because symptoms bleed into each other. A swollen joint might be arthritis-or just early scleroderma. Fatigue could be lupus-or muscle inflammation. A dry cough? Could be a cold. Or it could be lung scarring.
And here’s the kicker: many doctors aren’t trained to look for combinations. They’re trained to treat one disease at a time. So if you have lupus and your rheumatologist doesn’t check your lungs, the interstitial lung disease slips through. If your pulmonologist doesn’t know you have joint pain, they treat the lungs but miss the root cause.
How Autoantibodies Reveal the Truth
Blood tests aren’t just supportive-they’re the linchpin. In single autoimmune diseases, antibodies help confirm a diagnosis. In overlap syndromes, they’re often the only thing that makes the diagnosis.Anti-U1-RNP? If it’s above 1:10,000, and you have Raynaud’s, puffy hands, and arthritis, you’ve got MCTD. That’s not a guess. That’s a diagnostic threshold.
Anti-Jo-1? If you have muscle weakness and lung disease, this antibody is your smoking gun. Its specificity is 98%. That means if you have it, you almost certainly have antisynthetase syndrome-even if your symptoms don’t perfectly match the textbook.
Anti-PM/Scl? It’s rare, but when it’s present, it’s nearly always correct. Its specificity is 99%. One positive test can change your entire treatment plan.
But here’s the danger: some doctors order a full autoimmune panel and get lost in the noise. Not every positive antibody means disease. The trick is matching the antibody to the clinical picture. A positive ANA alone? Common. A positive anti-U1-RNP with swollen fingers and lung changes? That’s a syndrome.
What Treatment Actually Looks Like
There’s no one-size-fits-all treatment. You can’t just give prednisone and call it a day. You have to treat multiple diseases at once-and avoid making one worse while fixing another.The standard start is low-dose steroids (like prednisone) plus one immunosuppressant. Methotrexate is common. Mycophenolate mofetil is preferred if lung disease is involved. But if your lungs are failing, you need something stronger. Rituximab, a drug that targets B-cells, has shown 60-70% success in stabilizing lung function in antisynthetase syndrome. In 2023, the FDA approved tocilizumab for this exact use.
But here’s where things get risky: 35% of patients with overlap syndromes are on three or more immunosuppressants. That’s a lot. Your risk of serious infection jumps from 15% on one or two drugs to 28% on three. Pneumonia, sepsis, even tuberculosis can sneak in when your immune system is this suppressed.
And drug interactions? They’re common. Methotrexate and mycophenolate both stress the liver. Steroids raise blood sugar. If you’re also on thyroid meds or diabetes drugs, things get complicated fast.
That’s why treatment isn’t just about drugs. It’s about timing. You don’t treat all symptoms at once. You prioritize. If your lungs are failing, you focus there first. If your skin is tightening and limiting movement, you target that. Your treatment plan should shift as your disease shifts.
The Real Problem: Fragmented Care
The biggest obstacle isn’t medicine. It’s the system.You see a rheumatologist for your joints. A pulmonologist for your lungs. A dermatologist for your skin. A gastroenterologist for your dry mouth and eyes. Each visit is 15 minutes. Each doctor has a piece of your chart. No one has the full picture.
Patients report that 68% of those with Sjögren’s-lupus overlap struggle to get coordinated care. That’s not just inconvenient-it’s dangerous. Missed appointments. Conflicting advice. Medications that clash. Emergency room visits because no one saw the warning signs.
But there’s a better way. Centers like Johns Hopkins, Mayo Clinic, and Hospital for Special Surgery have built dedicated overlap syndrome programs. They don’t just have specialists. They have care coordinators. One person tracks your appointments, your labs, your medications, your symptoms. They schedule all your visits in one week. They call your specialists when something changes. They make sure your treatment plan is unified.
The results? 35% fewer hospitalizations. 42% better medication adherence. Patients report feeling heard for the first time.
What’s Changing Now
The field is waking up. In 2023, the NIH launched a $15 million project to find biomarkers that predict who will develop overlap syndromes-and which ones will progress fastest. AI tools are already being tested to scan electronic health records and flag patients at risk 12 months before symptoms show up.New treatment goals are emerging. Instead of just “control symptoms,” doctors are now aiming for specific targets: keep lung function above 80% of predicted, keep skin thickening below a certain score, maintain minimal disease activity in joints. These aren’t just nice ideas. They’re measurable outcomes.
And the pipeline is growing. Anifrolumab, a drug approved for lupus, is now in phase 2 trials for MCTD. New drugs targeting specific immune pathways are being designed for overlap syndromes, not just single diseases.
But progress depends on awareness. If you’re a patient with multiple symptoms that don’t fit one diagnosis, push for a rheumatologist who specializes in connective tissue diseases. If you’re a doctor, ask: Could this be more than one thing? Don’t stop at the first label.
What Patients Need to Know
If you suspect you have an overlap syndrome:- Keep a detailed symptom log-what hurts, when, and how bad.
- Ask for specific antibody tests: anti-U1-RNP, anti-Jo-1, anti-PM/Scl.
- Insist on a pulmonary function test and high-res CT scan if you have any breathing issues.
- Seek out a center with a dedicated autoimmune or overlap syndrome program.
- Ask if you have a care coordinator. If not, request one.
- Don’t accept “we don’t know” as an answer. Say: “What if I have more than one thing?”
Autoimmune overlap syndromes aren’t rare. They’re underdiagnosed. And they’re treatable-if you get the right team, the right tests, and the right plan.
Can you have more than one autoimmune disease at once?
Yes. When a person meets diagnostic criteria for two or more autoimmune diseases like lupus, scleroderma, myositis, or Sjögren’s, it’s called an autoimmune overlap syndrome. These aren’t random coincidences-they follow specific patterns tied to unique autoantibodies and clinical features. About 25% of people with one connective tissue disease will develop features of another within 5 to 10 years.
What are the most common autoimmune overlap syndromes?
The three most common are: Mixed Connective Tissue Disease (MCTD), linked to anti-U1-RNP antibodies and features of lupus, scleroderma, and myositis; Antisynthetase Syndrome, tied to anti-Jo-1 and marked by muscle weakness and lung scarring; and Polymyositis/Scleroderma (PM/Scl) overlap, defined by anti-PM/Scl antibodies and a mix of skin tightening and muscle inflammation. Each has a distinct antibody signature and clinical profile.
Why is diagnosis so difficult for overlap syndromes?
There are no official diagnostic criteria for overlap syndromes-only for the individual diseases they combine. Symptoms often look like one condition but are actually signs of multiple. Doctors may treat the most obvious symptom and miss the others. As a result, patients often wait 18 months or longer for a correct diagnosis, compared to 12 months for single autoimmune diseases.
Are blood tests enough to diagnose an overlap syndrome?
No. Blood tests are critical, but they must match your symptoms. A positive anti-U1-RNP antibody with Raynaud’s, puffy hands, and arthritis confirms MCTD. But a positive ANA alone is common in healthy people. The key is combining specific antibodies with clinical signs. Anti-Jo-1 with muscle weakness and lung disease? That’s antisynthetase syndrome. The antibody doesn’t stand alone-it completes the picture.
What’s the biggest risk in treating overlap syndromes?
The biggest risk is overtreating. Many patients end up on three or more immunosuppressants to manage different parts of their disease. This increases the chance of serious infections-from pneumonia to tuberculosis-from 15% with one or two drugs to 28% with three or more. Careful balancing is needed: treat the most dangerous component first, avoid unnecessary drugs, and monitor closely for side effects.
How important is coordinated care in managing overlap syndromes?
It’s essential. Patients who see multiple specialists without a care coordinator often face conflicting advice, missed appointments, and dangerous drug interactions. Centers with dedicated care coordinators-people who manage all appointments, labs, and communication between doctors-see 35% fewer hospitalizations and 42% better medication adherence. If you have multiple autoimmune conditions, ask if your clinic has a care coordination program.





Comments (16)