Digoxin has been used for over 200 years to treat heart failure and certain irregular heartbeats. It’s old, cheap, and effective-but it’s also one of the most dangerous drugs in common use. A tiny mistake in dosage, a change in kidney function, or even eating a grapefruit can push a patient into toxic territory. That’s why monitoring digoxin levels isn’t just good practice-it’s life-saving.
What happens when digoxin levels go wrong?
Digoxin works by slowing the heart rate and strengthening each beat. But the difference between the right dose and a toxic one is razor-thin. The therapeutic range is 0.5 to 2.0 ng/mL. Go above 2.0, and you’re in danger. Above 3.0, and you’re looking at potentially fatal heart rhythms.
Early signs of digoxin toxicity aren’t dramatic. Patients might feel nauseous, lose their appetite, or see halos around lights. These symptoms get mistaken for the flu, food poisoning, or aging. By the time confusion or irregular heartbeat shows up, it’s often too late. In Australia, digoxin toxicity accounts for over 2,000 emergency department visits each year. About 1 in 10 of those cases require hospitalization.
Who needs digoxin level checks the most?
Not everyone on digoxin needs weekly blood tests. But some groups are at much higher risk:
- Patients over 65-kidneys slow down with age, and digoxin is cleared mostly by the kidneys.
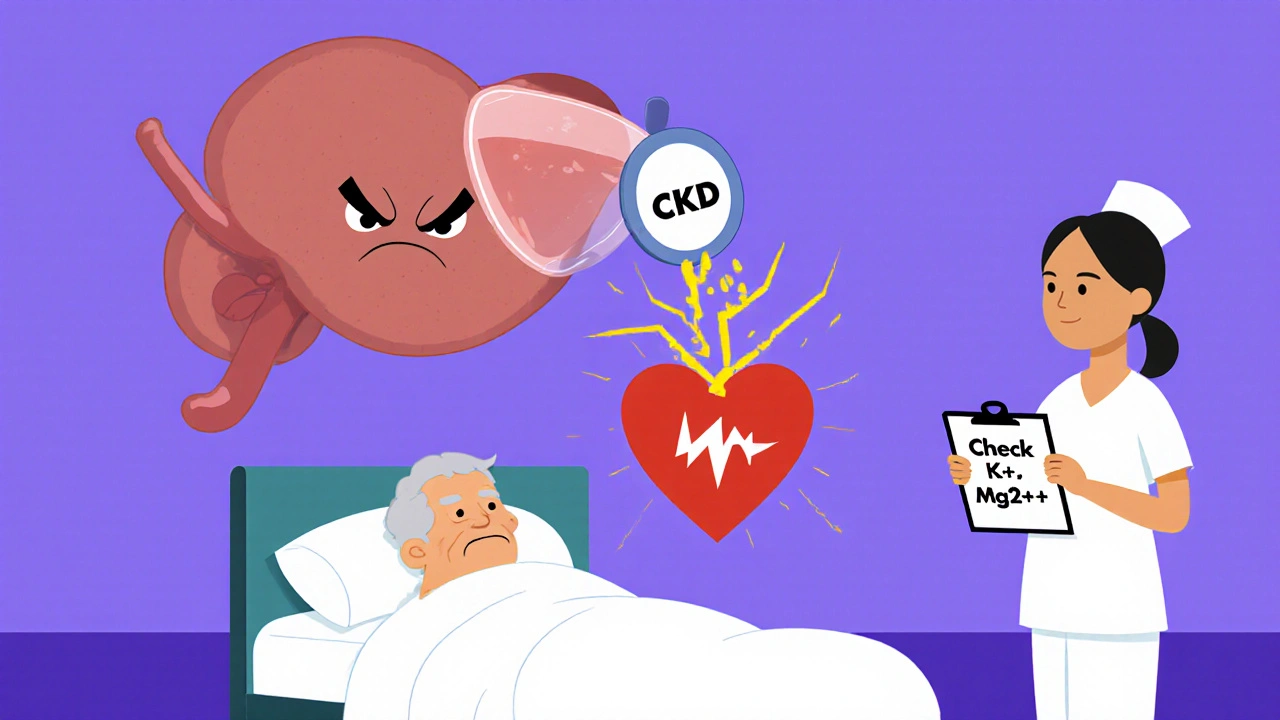
- People with kidney disease-even mild CKD increases toxicity risk by 300%.
- Those taking diuretics like furosemide-these drugs lower potassium and magnesium, which makes the heart more sensitive to digoxin.
- Patients on multiple medications-drugs like amiodarone, verapamil, or even some antibiotics can spike digoxin levels by blocking its clearance.
- Anyone who’s had recent illness, vomiting, or dehydration-fluid loss concentrates digoxin in the blood.
For these patients, levels should be checked within 5 to 7 days after starting or changing the dose, then every 3 to 6 months if stable. If they get sick or start a new drug, test again immediately.
When and how should digoxin levels be tested?
Digoxin levels aren’t useful if drawn at the wrong time. The blood test must be taken at least 6 to 8 hours after the last dose. Drawing it too soon gives a falsely high reading. Drawing it right before the next dose-trough level-is the standard.
The test itself is simple: a standard blood draw. But the timing and interpretation matter. A level of 1.8 ng/mL might be fine for a young, healthy person. For a frail 80-year-old with mild kidney impairment, that same level could be dangerous. Always interpret results in context: age, kidney function, electrolytes, and other meds.
Doctors often forget to check potassium and magnesium when digoxin levels are high. Low potassium (hypokalemia) makes digoxin toxicity 5 times more likely. Low magnesium? Even worse. Both need correction before adjusting the digoxin dose.
Common mistakes that lead to toxicity
Here are the most frequent errors seen in clinics and hospitals:
- Assuming a stable dose doesn’t need monitoring. Patients change. Kidneys decline. Weight drops. Meds change. No dose is forever.
- Not checking levels after starting a new drug. Amiodarone can double digoxin levels in weeks. Many prescribers don’t know this.
- Ignoring symptoms. Nausea or blurred vision? Not "just aging." It’s a red flag.
- Using the wrong reference range. Some labs still use outdated ranges (0.5-2.0 ng/mL). Newer evidence suggests the safest range is 0.5-1.0 ng/mL for elderly patients.
- Skipping follow-up. A patient gets a level checked once and never again. That’s like checking your car’s oil once and never again.
One study from the Royal Melbourne Hospital found that 68% of digoxin toxicity cases were preventable. Most happened because no one checked the levels after a change in the patient’s condition.
What to do if toxicity is suspected
If a patient has symptoms and a high digoxin level:
- Stop digoxin immediately.
- Check electrolytes-especially potassium, magnesium, and calcium.
- Get an ECG. Look for slow heart rate, heart block, or unusual rhythms like ventricular tachycardia.
- Call poison control or a toxicologist. Digoxin-specific antibody fragments (Digibind) are available and can reverse life-threatening toxicity within hours.
- Don’t give more digoxin to "counteract" the symptoms. That’s how people die.
Digibind isn’t cheap-it costs over $5,000 per vial-but it’s the only thing that works fast. Waiting for the body to clear digoxin naturally can take days. In a toxic patient, days are too long.

How to stay safe: a simple checklist
If you’re managing someone on digoxin, use this checklist:
- Confirm the patient’s kidney function (eGFR) every 3 months.
- Check digoxin levels 1 week after starting or changing dose.
- Test levels again if they’re sick, dehydrated, or start a new medication.
- Always check potassium and magnesium when drawing digoxin levels.
- Keep the dose as low as possible-0.125 mg daily is often enough for older adults.
- Warn patients about grapefruit, antacids, and herbal supplements like licorice root.
- Document every level and every dose change. If it’s not written down, it didn’t happen.
Why this matters more than you think
Digoxin isn’t going away. It’s still used in about 1 in 100 older adults with heart failure. But with newer drugs like SGLT2 inhibitors and ARNIs becoming first-line, digoxin is now a backup. That makes it even more dangerous. Doctors are less familiar with it. Nurses forget to monitor. Patients don’t know the risks.
Every time a patient on digoxin walks into a clinic, there’s a silent question: Is this level safe? If you don’t know the answer, you’re gambling with their life.
Monitoring digoxin levels isn’t bureaucracy. It’s the difference between a patient going home and a patient going to the ICU. It’s not about being perfect-it’s about being consistent. One test, one check, one question can save a life.
How often should digoxin levels be checked?
For new patients or after a dose change, check levels 5 to 7 days later. Once stable, check every 3 to 6 months. Test immediately if the patient gets sick, starts a new medication, or shows symptoms like nausea, vision changes, or irregular heartbeat. Elderly patients and those with kidney disease need more frequent checks.
Can digoxin toxicity be reversed?
Yes. Digoxin-specific antibody fragments (Digibind) bind to digoxin in the blood and neutralize it. This can reverse life-threatening toxicity within hours. It’s used in cases of severe arrhythmias, very high levels (above 3.0 ng/mL), or when symptoms are present. Supportive care like correcting electrolytes is also critical.
What drugs interact with digoxin?
Many common drugs raise digoxin levels. These include amiodarone, verapamil, diltiazem, clarithromycin, cyclosporine, and quinidine. Even over-the-counter antacids with magnesium or aluminum can reduce digoxin absorption if taken at the same time. Always review all medications when starting or adjusting digoxin.
Is digoxin still used today?
Yes, but less often. Newer drugs like SGLT2 inhibitors and ARNIs are now first-line for heart failure. Digoxin is typically reserved for patients with persistent symptoms despite other treatments, or those with atrial fibrillation needing heart rate control. It’s a second-line option-but because it’s cheap and effective, it’s still widely prescribed.
What’s the safest digoxin dose for older adults?
For most older adults, 0.125 mg once daily is the safest starting and maintenance dose. Many patients do well on this-even those with mild kidney impairment. Higher doses (0.25 mg) increase toxicity risk without adding much benefit. Always start low and go slow.





Comments (13)