When your insurance plan suddenly stops covering your medication, it’s not just a paperwork issue-it’s a health crisis. Imagine taking Humira for Crohn’s disease for seven years, paying $50 a month, then waking up one day to find your plan moved it to a non-preferred tier. Your cost jumps to $650. No warning. No easy fix. This isn’t rare. In 2024, 34% of Medicare beneficiaries experienced unexpected formulary changes affecting their drugs. And for many, the confusion around appeals, alternatives, and deadlines made things worse.
What Is a Formulary, Really?
A formulary is your insurance plan’s list of covered prescription drugs. It’s not just a catalog-it’s a decision engine. Every drug on the list is placed into a tier, and each tier has a different cost to you. Tier 1? Usually generics, maybe $5 to $15. Tier 3 or 4? Brand-name drugs, maybe $50 to $200. Tier 5? Specialty drugs like biologics for rheumatoid arthritis or multiple sclerosis-sometimes hundreds or even over $1,000 a month. Formularies aren’t random. They’re built by Pharmacy and Therapeutics (P&T) committees that review clinical data, cost-effectiveness, and manufacturer rebates. In 2024, 92% of Medicare Part D plans and 87% of commercial plans used a tiered formulary. That means your out-of-pocket cost isn’t just about the drug-it’s about where your drug sits on the list. And here’s the catch: formularies change. All the time. New drugs get added. Older ones get moved. Sometimes they’re removed entirely. The goal? Cut costs. But the impact? It lands on you.Why Formularies Change-and When You’ll Find Out
Plans don’t flip switches overnight. Changes happen through formal reviews, usually quarterly. Large pharmacy benefit managers (PBMs) like Express Scripts and Optum Rx review formularies every three months. But here’s where things get messy: you won’t always be told in time. Medicare Part D plans are required to give you 60 days’ notice before removing a drug or changing its tier. Commercial plans? Not so much. On average, you get 22 days. That’s barely enough to call your doctor, check alternatives, or file an exception. And according to a 2024 CAQH survey, 57% of patients say they got little to no warning. Why the gap? Commercial plans prioritize flexibility. They negotiate rebates with drugmakers-so if a company stops offering a big discount, the drug gets bumped up in cost or dropped. It’s business. But for you, it’s your treatment.What Happens When Your Drug Gets Dropped
Let’s say your insulin, your asthma inhaler, or your blood pressure pill suddenly isn’t covered anymore. What do you do? First, don’t stop taking it. Stopping suddenly can cause hospital visits. In fact, a 2023 Scripta Insights report found that 18% of patients quit their meds after a coverage change-leading to more ER trips and higher long-term costs. Here’s your action plan:- Check your plan’s formulary-right now. Use your insurer’s website or app. Search your drug by name. Look for changes in tier, prior authorization, or step therapy requirements.
- Ask your doctor-not just for a replacement, but for a therapeutic alternative. Is there another drug in the same class that’s on your plan? For example, if your brand-name lisinopril was dropped, is generic lisinopril still covered? (Spoiler: usually yes.)
- Request a formulary exception. This is a formal appeal. You need your doctor to submit a letter saying the change would harm your health. CMS data shows 64% of medically justified exceptions get approved.
- Look into manufacturer assistance. Companies like AbbVie (Humira), Roche (Ocrevus), and Novo Nordisk (Ozempic) have patient support programs. In 2024, they covered $6.2 billion in out-of-pocket costs for patients.
- Use GoodRx or SingleCare. Even if your insurance won’t cover it, these apps can show cash prices that are lower than your copay. For some specialty drugs, the cash price is cheaper than your tier 4 copay.

Medicare vs. Commercial Plans: The Big Differences
If you’re on Medicare Part D, you have more protections. The government requires:- At least two drugs per therapeutic class
- 60 days’ notice for non-urgent changes
- 72-hour turnaround on urgent exception requests
- 30-60 day transition periods if your drug is removed
How Providers Can Help You Stay Covered
Good doctors don’t just write prescriptions-they track formularies. Large medical groups now use e-prescribing systems that check your plan’s formulary in real time. When your doctor sends a script, the system says: “This drug is tier 3. Here’s a tier 1 alternative. Would you like to switch?” That’s proactive. And it works. 76% of large practices use this tech. But if you’re seeing a smaller clinic, don’t assume they’re doing it. Ask: “Is this drug covered under my plan?” Show them your card. Or better yet, log into your plan’s website and give them the formulary tier number.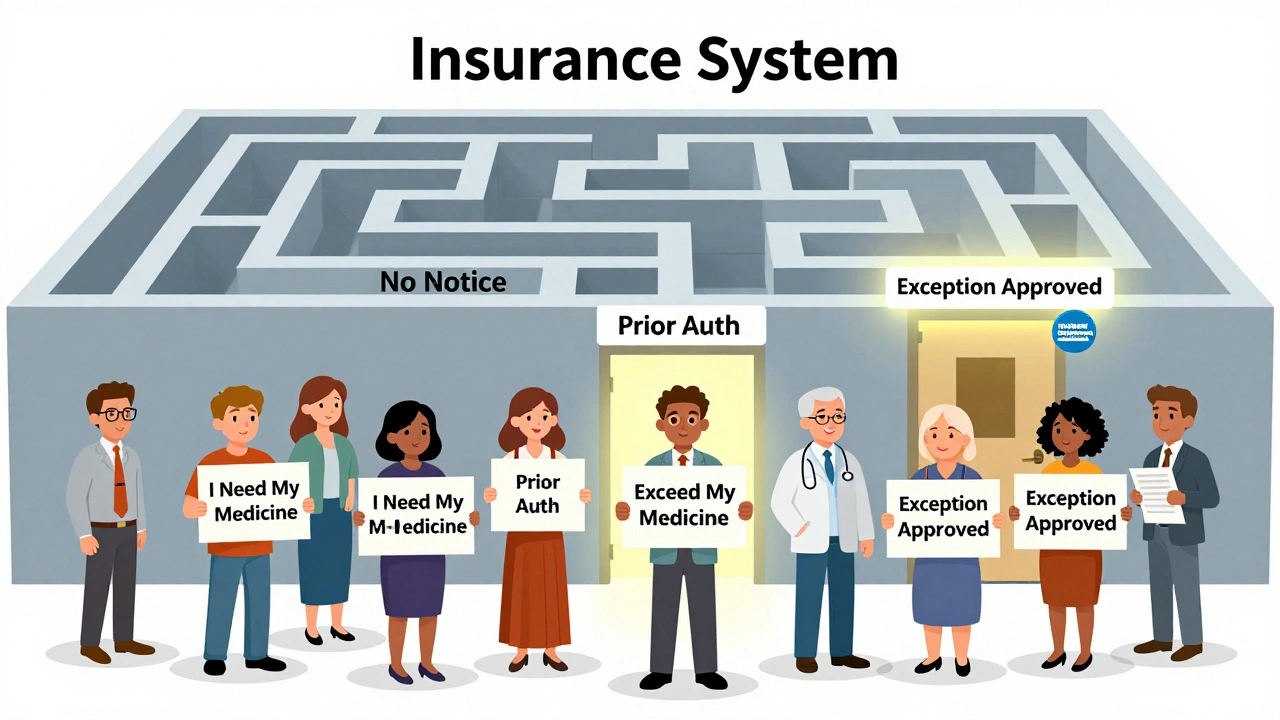
What You Can Do Before It Happens
Don’t wait for a surprise. Be the person who checks before it’s too late.- During open enrollment (October 15-December 7 for Medicare, anytime for commercial), compare formularies. Don’t just look at premiums. Look at your drugs.
- After major life events-job change, divorce, turning 65-recheck coverage. Your new plan might not cover what your old one did.
- Sign up for plan alerts. Most insurers let you opt into email or text alerts about formulary changes.
- Keep a list of all your meds, dosages, and why you take them. If you need an exception, you’ll need this.
The Future: Personalized Formularies and AI
The next wave of formulary management won’t just be about cost. It’s about predictability. AI tools now analyze your history-your adherence, your lab results, your side effects-and predict which drugs you’re likely to stick with. Some plans are testing individualized formularies based on genetic data and past response. By 2027, 45% of employer plans are expected to use value-based formularies-where the drug’s real-world outcomes matter more than its list price. If a drug keeps you out of the hospital, it stays on the list. If it doesn’t, it gets replaced. But here’s the problem: only 22% of patients understand how these decisions are made. That’s not transparency. That’s a gap.Final Reality Check
Formularies aren’t going away. They’re the engine behind $600 billion in annual drug spending. But they’re not perfect. They can save money. They can also hurt people. The key isn’t to fight the system-it’s to navigate it. Know your plan. Know your drugs. Know your rights. And if your medication gets pulled, act fast. You have options. You just need to use them before it’s too late.What should I do if my insurance stops covering my medication?
First, don’t stop taking it. Contact your doctor to ask for a therapeutic alternative that’s still covered. Then, file a formulary exception request with your insurer-your doctor must support it with a letter explaining why the change would harm your health. You can also check manufacturer assistance programs or use cash-price apps like GoodRx. Most plans approve exceptions if there’s clear medical need.
How much notice do I get before a formulary change?
Medicare Part D plans must give you 60 days’ notice for non-urgent changes. Commercial plans have no federal requirement-most give 22 days on average. Some give as little as 10. Always check your plan’s website or sign up for email alerts. Don’t wait for a letter.
Can I switch plans if my drug gets dropped?
If you’re on Medicare, you can switch during the Annual Enrollment Period (October 15-December 7) or during a Special Enrollment Period if you qualify (like moving or losing other coverage). For commercial plans, you usually can’t switch mid-year unless you have a qualifying life event. Your best move is to request an exception or find a covered alternative.
Why are some drugs on tier 4 or 5 even if they’re generic?
Sometimes, a generic drug is placed in a higher tier if it’s newer, more expensive to produce, or if the manufacturer didn’t offer a good rebate. Other times, it’s because the plan wants to steer you toward an even cheaper alternative. Tier placement isn’t always about the drug’s cost-it’s about what the insurer can negotiate.
What’s the difference between a formulary exception and a prior authorization?
Prior authorization means your doctor needs approval before the plan will cover the drug-usually because it’s expensive or has safety concerns. A formulary exception is when a drug isn’t on your plan’s list at all, and you’re asking them to make an exception. Both require a doctor’s note, but exceptions are harder to get because you’re asking them to cover something they explicitly excluded.
Are there free resources to help me understand my formulary?
Yes. Medicare beneficiaries can call State Health Insurance Assistance Programs (SHIP) for free, one-on-one help. Many states have local SHIP offices. For commercial plans, your insurer’s customer service line should help you decode your formulary. You can also use tools like Medicare’s Plan Finder or GoodRx to compare coverage.






Comments (13)