If you’ve ever been told your doctor needs to wait for insurance to approve your medication before you can fill it, you’ve run into prior authorization. It’s not a glitch. It’s not a mistake. It’s a standard step in how most health plans control costs - and it’s happening more often than you think.
What Is Prior Authorization?
Prior authorization, sometimes called pre-authorization or pre-certification, is when your health plan requires your doctor to get approval before they can prescribe certain medications. It’s not about denying care. It’s about making sure the right drug is used for the right reason - and that it’s the most cost-effective option available. Prior authorization is a process used by insurance companies to review whether a prescribed medication meets specific clinical and financial criteria before covering it. It’s part of managed care pharmacy practices designed to balance patient safety with cost control. Under Medicare Part D, it’s officially called a “coverage determination.” This isn’t just for expensive drugs. Even common brand-name medications with cheaper generic versions often require it. Your plan doesn’t automatically cover everything on the pharmacy shelf. They’ve built a list - called a formulary - of what they’ll pay for, and prior authorization is the gatekeeper for drugs that fall outside the usual rules.Why Does It Exist?
You might wonder: why make doctors jump through hoops just to prescribe a pill? The short answer: money. And safety. Insurance companies use prior authorization to avoid paying for drugs that:- Have cheaper, equally effective alternatives (like generics)
- Are high-cost with unclear benefits
- Are used in ways not approved by the FDA (off-label)
- Could interact dangerously with other medications you’re taking
- Have a risk of abuse or addiction
Which Medications Usually Need Prior Authorization?
Not every drug needs approval. But these categories almost always do:- Brand-name drugs with generic equivalents - like Lipitor vs. atorvastatin
- High-cost specialty medications - think biologics for rheumatoid arthritis or hepatitis C
- Drugs with strict usage rules - for example, only approved for patients who failed two other treatments first
- Medications with abuse potential - opioids, stimulants, benzodiazepines
- Off-label uses - when a drug is prescribed for a condition not listed on its FDA label
How Does the Process Work?
It’s not complicated - but it’s slow. Here’s the step-by-step:- Your doctor decides you need a medication that requires prior authorization.
- They check your plan’s formulary and confirm the requirement.
- They fill out a form - either online, by fax, or through an electronic system - explaining why you need this specific drug. They must include your diagnosis, medical history, and why alternatives won’t work.
- The insurance company reviews the request. This can take 24 hours for urgent cases or up to 14 days for standard requests.
- You get a call or letter: approved or denied.
- If approved, the authorization lasts for a set time - usually 6 to 12 months. After that, your doctor must reapply.
What Happens If It’s Denied?
Denials happen. About 1 in 5 prior authorization requests are initially rejected - often because the paperwork was incomplete or the doctor didn’t explain the medical necessity clearly enough. You have rights. If your request is denied:- Your doctor can appeal. They’ll submit more evidence - lab results, specialist notes, even published studies supporting the drug’s use.
- You can file your own appeal directly with the insurer. Medicare and most commercial plans require them to respond within 30 days.
- If it’s an emergency or life-threatening situation, prior authorization isn’t required. But you still need to notify your plan within 48 hours.
What Can You Do to Speed It Up?
You’re not powerless in this process. Here’s how to help:- Ask upfront. Before your doctor writes the prescription, ask: “Does this need prior authorization?”
- Check your plan’s website. Most insurers have a formulary search tool. Type in the drug name and see if it says “prior auth required.”
- Ask about alternatives. If your drug needs authorization, ask your doctor: “Is there another option that’s covered without extra steps?”
- Use urgent requests. If you’re out of meds and your condition is worsening, your doctor can mark the request as “urgent.” This often cuts approval time to 24 hours.
- Pay out-of-pocket temporarily. If you can afford it, buy the medication now and submit a claim later for reimbursement once approved. GoodRx says this is a common workaround.
Who’s Responsible?
Many patients think, “It’s the doctor’s job.” And technically, yes - they submit the paperwork. But you’re the one who gets stuck without meds if it’s delayed. So you’re the most important person in this process. Mayo Clinic says patients are responsible for knowing their coverage. Don’t assume your insurance will cover it. Don’t wait until you get to the pharmacy to find out. Call your insurer. Check your plan’s website. Keep a list of your medications and their prior auth status.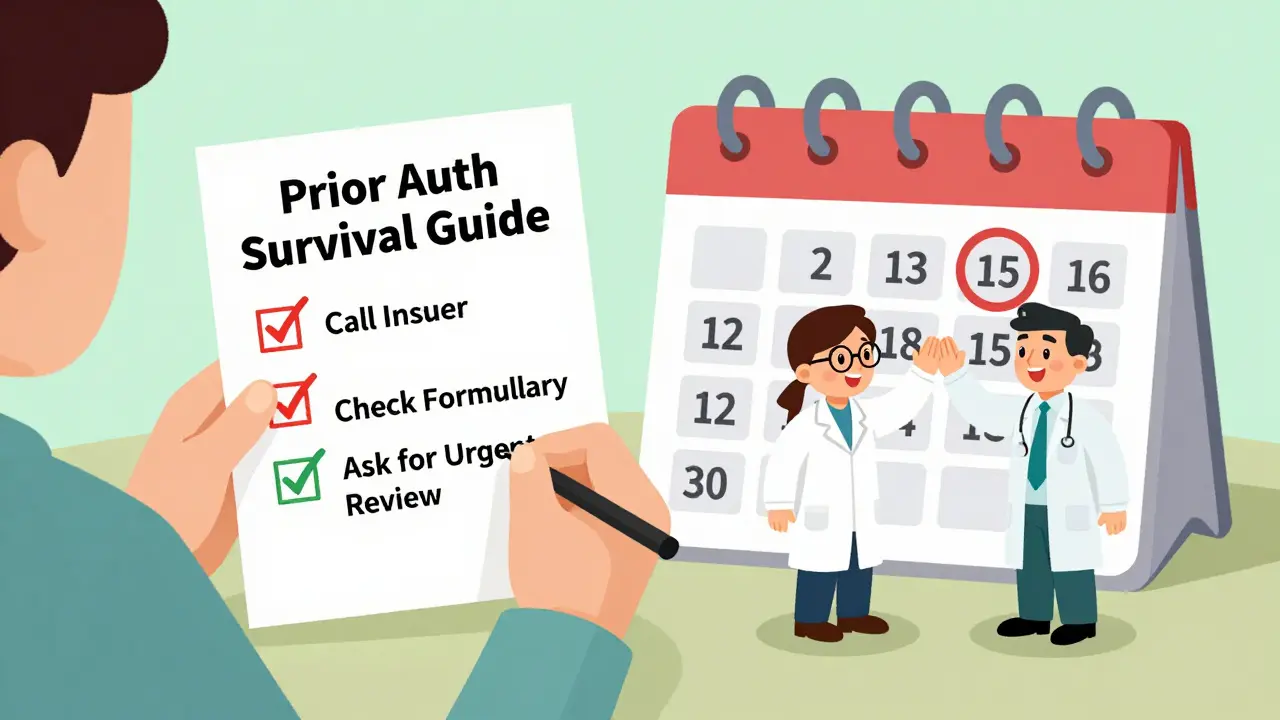
Is This Going Away?
No. And it’s not just in the U.S. - similar systems exist in Canada, Australia, and the UK, though they’re less common in public systems. The American Medical Association (AMA) calls prior authorization a “tactic used by insurers to control costs.” Doctors hate it. They spend an average of 15 hours a week on paperwork just to get prescriptions approved. But insurers won’t drop it. It saves billions. A 2023 study by the Academy of Managed Care Pharmacy found prior authorization helped reduce unnecessary spending on high-cost drugs by up to 22% in some plans. The real issue isn’t whether it exists - it’s how broken the system is. Long delays. Confusing forms. Lack of communication. Patients suffer the most.What’s Next?
You can’t control the system - but you can master it.- Keep a printed or digital list of your medications and which ones need prior authorization.
- Set calendar reminders for when authorizations expire.
- Always ask your pharmacist: “Is this covered?” before you pay.
- If you’re switching plans, check the new formulary before you enroll.
What happens if I don’t get prior authorization for my medication?
If you don’t get prior authorization and your insurance requires it, your pharmacy won’t be able to bill your plan. You’ll have to pay the full price out-of-pocket - which can be hundreds or even thousands of dollars for specialty drugs. Even if you later get approved, your plan won’t reimburse you retroactively unless you file a claim and meet their deadlines.
Can I get a 90-day supply with prior authorization?
Yes - but only if your plan allows it and the prior authorization covers a 90-day supply. Most plans prefer 30-day fills unless you’re on a maintenance medication (like blood pressure or diabetes drugs). Your doctor can request a 90-day authorization, but they’ll need to justify why it’s medically necessary - and your plan may require you to use a mail-order pharmacy.
Do Medicare Part D plans require prior authorization?
Yes. Medicare Part D plans use prior authorization - which they call “coverage determination” - for many high-cost and specialty drugs. You’ll get a notice if your drug needs approval. You or your doctor can appeal a denial, and Medicare requires them to respond within 72 hours for urgent cases and 7 days for standard requests.
Can my doctor prescribe any medication if I’m on Medicare?
Your doctor can prescribe any medication, but Medicare Part D plans decide what they’ll pay for. Even if your doctor says a drug is right for you, your plan can still deny coverage unless the drug is on their formulary and you get prior authorization - if required. That’s why it’s important to check your plan’s formulary before your doctor writes the prescription.
Is prior authorization the same as a prior authorization exception?
No. A prior authorization is the standard request for coverage. A prior authorization exception - sometimes called a “formulary exception” - is when you ask your plan to cover a drug that’s not on their list at all. This requires even more documentation, like clinical studies or evidence that other covered drugs didn’t work. It’s harder to get approved, but it’s possible.
Final Tip: Stay Organized
Keep a folder - digital or physical - with:- Names of medications that require prior authorization
- Approval dates and expiration dates
- Phone numbers for your insurer’s pharmacy line
- Notes from your doctor about why each drug was chosen





