Statin Tolerance Assessment Tool
Symptom Assessment
Other Potential Causes
Your Assessment Results
What Really Happens When Statins Cause Muscle Pain?
Most people think if statins hurt their muscles, they just can’t take them anymore. But that’s not always true. Around 7 to 29% of people on statins say they feel sore, weak, or tired-especially in their thighs or shoulders. But here’s the catch: only about 5 to 15% of those people actually have statin-associated muscle symptoms (SAMS). The rest? Their symptoms might be from something else-low vitamin D, an underactive thyroid, even just aging. That’s why specialized statin intolerance clinics exist. They don’t just say “stop the statin.” They figure out what’s really going on.
How Do These Clinics Work?
Statin intolerance clinics follow clear, step-by-step rules. It’s not guesswork. The process starts with stopping the statin completely for two weeks. During that time, patients track their symptoms: where the pain is, how bad it is (on a scale of 0 to 10), and whether it gets better without the drug. If the pain fades, that’s a clue. Then, doctors check for other causes-thyroid levels, vitamin D, kidney function, even alcohol or supplements like red yeast rice that can mimic statin side effects.
Once those are ruled out, the real test begins: rechallenge. Instead of going back to the same statin, patients try a different one. Not just any one-usually a hydrophilic statin like rosuvastatin or pravastatin. These don’t leak into muscle tissue the way lipophilic ones (like simvastatin or atorvastatin) do. They’re pulled straight into the liver, where they’re supposed to work. In clinics using this method, 72% of patients who thought they were intolerant ended up tolerating a new statin just fine.
What If You Still Can’t Tolerate Any Statin?
Some people really can’t take any statin, even at the lowest dose. That’s where the next step kicks in: non-statin options. The first go-to is ezetimibe. It’s cheap-about $35 a month-and proven to cut LDL cholesterol by 15-20% and reduce heart attacks by 6%, based on the IMPROVE-IT trial. For people who still need more, bempedoic acid (Nexletol) is a newer option. It works in the liver like statins but doesn’t enter muscle cells. In a trial with over 14,000 people, it lowered LDL by 18% with almost no muscle pain.
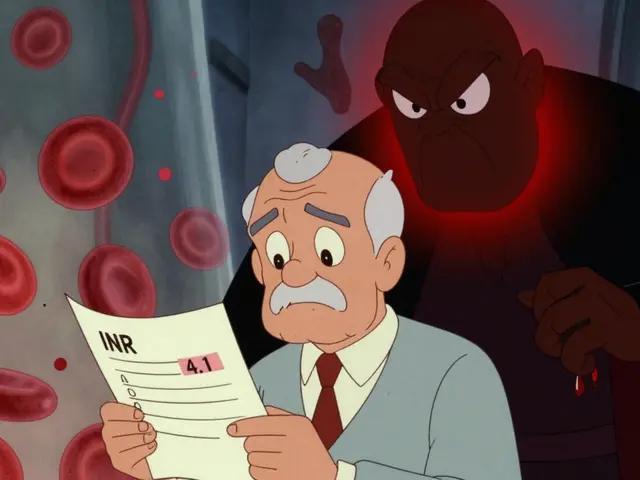
Then there’s the expensive but powerful option: PCSK9 inhibitors like evolocumab. They slash LDL by 50-60%, but cost around $5,850 a year. Insurance often fights covering them, even when patients qualify. That’s a big hurdle. That’s why clinics use tools like the ACC’s Statin Intolerance Tool, which helps doctors weigh the real risk of a heart attack against the cost and access barriers of alternatives.
Intermittent Dosing: A Game Changer for Many
One of the most surprising findings? You don’t always need to take a statin every day. Long-acting statins like rosuvastatin stick around in your body for days. So taking it just twice a week-say, Monday and Thursday-can still lower LDL by 20-40%. In a Cleveland Clinic study of 1,247 patients who couldn’t take statins daily, 76% tolerated this schedule without pain. One patient on Reddit, HeartPatient87, shared: “After five years of being told I was intolerant, I started rosuvastatin 5mg twice a week. My LDL dropped from 142 to 89. No pain.”
This approach isn’t just convenient-it’s backed by data. Clinics that use intermittent dosing see 18% of patients permanently quitting statins. In places without protocols, that number jumps to 45%. That’s a huge difference in long-term heart health.
Why Most Doctors Don’t Do This
Here’s the problem: most primary care doctors aren’t trained in this. They see a patient with muscle pain, say “stop the statin,” and move on. No rechallenge. No testing for other causes. No switching statins. No intermittent dosing. That’s why patients end up stuck. The American College of Cardiology found that 42% of community hospitals have no formal protocol for statin intolerance. Only 87% of academic medical centers do.
It’s not that doctors don’t care. They’re busy. They don’t have time to dig into muscle symptoms. That’s where statin intolerance clinics step in. They’re staffed with lipid specialists, pharmacists, and dietitians who do nothing but manage these cases. At Cleveland Clinic, pharmacists lead the rechallenge process-and their patients have 22% better outcomes than those managed by doctors alone.

What Patients Are Saying
People who’ve been through these clinics say the same thing: “I thought I had no options.” One patient on the Inspire forum spent 11 weeks appealing insurance denials to get PCSK9 inhibitors approved. Another said, “My local hospital told me to live with high cholesterol. The lipid clinic gave me back my life.” Kaiser Permanente’s internal survey found 82% of patients in their program were able to restart lipid-lowering therapy-compared to just 45% elsewhere.
But it’s not perfect. Wait times for appointments are long-6 to 8 weeks on average. And even when a clinic finds a solution, insurance often blocks the next step. That’s why success isn’t just about the protocol. It’s about advocacy, persistence, and knowing your rights.
The Future Is Here-And It’s Personalized
Things are changing fast. Mayo Clinic now tests for the SLCO1B1 gene variant, which tells you if you’re genetically more likely to get muscle pain from simvastatin. That’s a game-changer. If you have the variant, you avoid simvastatin entirely. No trial and error.
Even more exciting? New statin formulations are in trials. One nanoparticle-delivered version, currently in phase 2, showed 92% tolerability in early tests. That means the drug is wrapped in a tiny capsule that delivers it straight to the liver, skipping the muscles entirely.
And the guidelines are catching up. The National Lipid Association updated its definition in 2022 to focus on symptoms, not just blood tests. The ACC’s Statin Intolerance Tool, launched in March 2023, is now used in over 600 clinics. It’s not just a checklist-it’s a decision engine. It asks: What’s your 10-year heart attack risk? How bad are your symptoms? What’s your budget? Then it recommends the safest, most effective path.
What You Can Do Right Now
If you’ve been told you’re statin intolerant and you’re still worried about your heart:
- Don’t assume you’re stuck. Ask for a rechallenge with a different statin.
- Request tests for vitamin D, thyroid function, and creatine kinase (CK) levels.
- Ask about intermittent dosing-especially with rosuvastatin or pravastatin.
- Push for ezetimibe or bempedoic acid if statins still don’t work.
- Find a lipid specialist. They’re not just for rare cases-they’re for anyone who’s been written off.
Statin intolerance isn’t a dead end. It’s a puzzle. And with the right team, the right tests, and the right plan, most people can get back on track-without pain, without fear, and with real protection for their heart.
Can statin side effects be reversed?
Yes. Most muscle-related side effects from statins go away within 2 to 4 weeks after stopping the medication. This is why clinics require a two-week washout period before confirming intolerance. If symptoms don’t improve after stopping, another cause-like thyroid issues or vitamin deficiency-needs to be checked.
Is it safe to take statins every other day or twice a week?
For certain statins like rosuvastatin and atorvastatin, yes. These have long half-lives, meaning they stay active in your body for days. Studies show intermittent dosing (e.g., 5mg rosuvastatin twice a week) lowers LDL cholesterol by 20-40% and is tolerated by 76% of patients who previously couldn’t take statins daily. It’s not for everyone, but it’s a proven option when daily dosing causes side effects.
What’s the difference between lipophilic and hydrophilic statins?
Lipophilic statins (like simvastatin, atorvastatin, and lovastatin) easily pass into muscle tissue, which is why they’re more likely to cause muscle pain. Hydrophilic statins (like rosuvastatin and pravastatin) are pulled mainly into the liver by transporters and don’t spread as much into muscles. Switching from a lipophilic to a hydrophilic statin is the most common successful strategy in statin intolerance clinics.
How do I know if my muscle pain is really from statins?
True statin-associated muscle symptoms (SAMS) usually start 2-4 weeks after starting or increasing the dose. The pain is symmetric-both legs or both arms-and affects large muscles like thighs or shoulders. It improves within 2-4 weeks after stopping the statin. If pain starts right away, is one-sided, or doesn’t improve after stopping, it’s likely not from the statin. A structured rechallenge under medical supervision is the only way to confirm.
Are there alternatives to statins that actually work?
Yes. Ezetimibe lowers LDL by 15-20% and reduces heart attacks by 6%. Bempedoic acid (Nexletol) lowers LDL by 18% with almost no muscle side effects. PCSK9 inhibitors like evolocumab drop LDL by 50-60% and reduce heart attacks and strokes. These aren’t just supplements-they’re proven, FDA-approved medications with clinical trial data backing them. The key is matching the right one to your risk level and budget.
Why do some doctors say I’m just imagining the pain?
They’re not saying you’re imagining it-they may be saying the pain isn’t caused by the statin. Studies suggest up to 80% of patients who think they’re intolerant might actually tolerate statins if tested properly. This is called the nocebo effect: expecting side effects makes you more likely to notice them. That’s why clinics use blinded rechallenges when possible. It’s not about dismissing your experience-it’s about finding the real cause.
Can I get genetic testing for statin intolerance?
Yes, but it’s not routine yet. The SLCO1B1 gene variant increases the risk of muscle pain from simvastatin. Mayo Clinic and some academic centers now test for it. If you have the variant, you’re advised to avoid simvastatin entirely. The test doesn’t predict intolerance to all statins, but it can prevent unnecessary stopping of a drug that might still work for you.
How do I find a statin intolerance clinic near me?
Start by asking your cardiologist or primary care doctor for a referral to a lipid specialist. Most statin intolerance clinics are based in academic medical centers or large hospital systems. You can also check the National Lipid Association’s website for member clinics or search for “lipid clinic” + your city. If you’re in the U.S., many insurance plans now cover these visits under Medicare Part B and private plans since 2023.



Comments (15)